Do Fallen Arches Have To Have Surgery?
Overview
he belly isn't the only part of your body subject to middle-age spread. As we get older, the years of walking and standing can cause feet to spread and flatten out as ligaments that support the arch lose their holding power. The result: the condition known as fallen arches, or flat feet. "Keep in mind that we're talking about 26 bones in the foot that are supported by a series of ligaments, muscle tendons and other connective tissue," says Glenn Gastwirth, D.P.M., deputy executive director of the American Podiatric Medicine Association in Bethesda, Maryland. "Over a period of time, the ligaments stretch out or 'give' under the pressure of your weight-especially if you're overweight. So what usually happens is you go shopping for new shoes one day and suddenly realize that you now need a size 8 when you've always worn a size 6. You may think your foot has grown, but what really happens is that the foot has spread out, both in width and length."
Causes
An acute injury, such as from a fall, can tear the posterior tibial tendon or cause it to become inflamed. The tendon can also tear due to overuse. For example, people who do high-impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Once the tendon becomes inflamed or torn, the arch will slowly fall (collapse) over time. Posterior tibial tendon dysfunction is more common in women and in people older than 40 years of age. Additional risk factors include obesity, diabetes, and hypertension.
Symptoms
Structural problems in your feet like fallen arches can alter your walking pattern, running pattern and cause pain throughout your body. Clear and accurate assessment of the mechanics of your lower limbs is key to understanding the profound effect that subtle faults in your foot, ankle, knee and hip alignment can cause.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
arch support plantar fasciitis
Non Surgical Treatment
The simplest form of treatment is the use of custom fitted orthotics. For this, it is best to see a podiatrist, who is a trained medical professional that assesses feet and gives you a prescription for the orthotic. If the orthotics do not work - or if the deformity is very severe - then surgical management may be needed. There is a very wide range of procedures available, with varying downtimes and complexity. The simplest procedure of all is a simple calf release. This can be done at the back of the knee or the calf, and has a very quick recovery. It is a day-surgery procedure, and the patient can walk immediately after the surgery without the need for a cast. Recovery back to jogging can be as early as three weeks. The calf release stops the deforming force but obviously does not correct the arch itself. It is usually done in combination with some of the other procedures mentioned below. Done by itself, the patient will probably still require orthotics but by releasing the calf, it allows the orthotics to be much more effective. The other end of the spectrum is a complete reconstruction of the arch with bone work and screws to fuse joints.
Surgical Treatment

Rarely does the physician use surgery to correct a foot that is congenitally flat, which typically does not cause pain. If the patient has a fallen arch that is painful, though, the foot and ankle physicians at Midwest Orthopaedics at Rush may perform surgery to reconstruct the tendon and "lift up" the fallen arch. This requires a combination of tendon re-routing procedures, ligament repairs, and bone cutting or fusion procedures.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
he belly isn't the only part of your body subject to middle-age spread. As we get older, the years of walking and standing can cause feet to spread and flatten out as ligaments that support the arch lose their holding power. The result: the condition known as fallen arches, or flat feet. "Keep in mind that we're talking about 26 bones in the foot that are supported by a series of ligaments, muscle tendons and other connective tissue," says Glenn Gastwirth, D.P.M., deputy executive director of the American Podiatric Medicine Association in Bethesda, Maryland. "Over a period of time, the ligaments stretch out or 'give' under the pressure of your weight-especially if you're overweight. So what usually happens is you go shopping for new shoes one day and suddenly realize that you now need a size 8 when you've always worn a size 6. You may think your foot has grown, but what really happens is that the foot has spread out, both in width and length."
Causes
An acute injury, such as from a fall, can tear the posterior tibial tendon or cause it to become inflamed. The tendon can also tear due to overuse. For example, people who do high-impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Once the tendon becomes inflamed or torn, the arch will slowly fall (collapse) over time. Posterior tibial tendon dysfunction is more common in women and in people older than 40 years of age. Additional risk factors include obesity, diabetes, and hypertension.
Symptoms
Structural problems in your feet like fallen arches can alter your walking pattern, running pattern and cause pain throughout your body. Clear and accurate assessment of the mechanics of your lower limbs is key to understanding the profound effect that subtle faults in your foot, ankle, knee and hip alignment can cause.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
arch support plantar fasciitis
Non Surgical Treatment
The simplest form of treatment is the use of custom fitted orthotics. For this, it is best to see a podiatrist, who is a trained medical professional that assesses feet and gives you a prescription for the orthotic. If the orthotics do not work - or if the deformity is very severe - then surgical management may be needed. There is a very wide range of procedures available, with varying downtimes and complexity. The simplest procedure of all is a simple calf release. This can be done at the back of the knee or the calf, and has a very quick recovery. It is a day-surgery procedure, and the patient can walk immediately after the surgery without the need for a cast. Recovery back to jogging can be as early as three weeks. The calf release stops the deforming force but obviously does not correct the arch itself. It is usually done in combination with some of the other procedures mentioned below. Done by itself, the patient will probably still require orthotics but by releasing the calf, it allows the orthotics to be much more effective. The other end of the spectrum is a complete reconstruction of the arch with bone work and screws to fuse joints.
Surgical Treatment

Rarely does the physician use surgery to correct a foot that is congenitally flat, which typically does not cause pain. If the patient has a fallen arch that is painful, though, the foot and ankle physicians at Midwest Orthopaedics at Rush may perform surgery to reconstruct the tendon and "lift up" the fallen arch. This requires a combination of tendon re-routing procedures, ligament repairs, and bone cutting or fusion procedures.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
All You Ought To Understand About Heel Discomfort
Overview

The heel is the first bone to contact the ground when walking and takes the full force of impact and the resulting shock of bearing weight during motion. The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking. The most common cause of heel pain is plantar fasciitis. Plantar fasciitis is a stretching of the plantar fascia, a ligament that runs from the ball of foot through the arch and is attached to the heel. It is that attachment which becomes aggravated and typically causes pain after being on your feet for lengths of time. Abnormal motion of the foot (pronation) is one cause of plantar fasciitis. Heel spurs, which are abnormal bone growths coming off the heel, can also cause heel pain. Other causes include repetitive stress or shock to the heel, standing for prolonged periods or osteoarthritis. To prevent heel pain, always wear properly fitting shoes, place insoles or inserts in your shoes to help control abnormal foot motion, maintain a healthy weight, exercise and do foot stretches as they have been shown to decrease the incidence of heel pain.
Causes
Plantar fasciitis is caused by inflammation and irritation of the tight tissue forming the arch of the foot. The most common cause of heel pain, it typically affects men, aged 40 - 70 who are physically active. The bottom or inside of the foot and / or heel (where heel and arch meet) may hurt or cause severe pain upon standing after resting -- or most often, when arising in the morning. The pain is usually experienced within the first few steps and is often characterized as "walking on nails" or knife blades. The pain may let up after walking a bit but most commonly returns after prolonged movement or a rest.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
If the plantar fasciitis is acute, that is, a sprain of the plantar fascia then it is basically treated as a sprain, with anti-inflammatory drugs, ice, rest, possibly physical therapy. If chronic, the poor foot mechanics need be addressed. Foot mechanics are changed by use of specially moulded shoe inserts known as orthotics. Someone with plantar fasciitis needs an orthotic designed to relieve strain on the plantar fascia. Orthotics are often confused with arch supports. Arch supports, by holding up the arch can remove some of the tension from the plantar fascia. Orthotics, on the other hand, do most of their work on the heel and ball of the foot repositioning the foot for maximized function. What can you do before you see the foot doctor? First, try doing your own version of deep tissue massage by rolling a frozen cola bottle or can from the heel forward into the arch. Do it gently. Do stretching but the key to good stretching is not to stretch too hard so generally avoid weight bearing (standing) stretches but sit on a soft surface like your bed and pull the foot backward on the leg as far as it will go, holding for 20 seconds and relaxing for 5 seconds. Each 25 second ?set? can be repeated 5 times and you have invested about 2 minutes in giving yourself a lot of help. Watch out for the shoes you wear. It is tempting to obtain shoes that are colorful and soft. Here is the proof that soft shoes are bad. Wrap a pillow around your foot with duct tape and walk for a block or two. You will come back with your foot hurting more because your foot sank down deeper into the soft surface, allowing the ligament to stretch more. The shoes should be stiff in the shank and flexible at the ball. Such shoes, to running buffs, are known as motion control shoes or stability shoes so going to one of the small specialty running shoes stores is a good place to start. If you don?t have a desk job, or have an industrial job see if light duty is available. A note from your doc may be all that is required in most cases and most doctors are happy to oblige.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
heel cushions for plantar fasciitis
Prevention

Before you get out of bed in the morning, and then periodically throughout the day, do the following exercises to increase flexibility and ease pain. Slowly flex your foot and toes to stretch the tissue on the bottom of your sore foot. Hold the stretch for 10 counts. Relax and repeat. Do gentle ankle rolls to keep the tissues around the ankle and on the back of the heel flexible. Sit on the edge of your bed and roll your foot back and forth over a tennis ball.

The heel is the first bone to contact the ground when walking and takes the full force of impact and the resulting shock of bearing weight during motion. The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking. The most common cause of heel pain is plantar fasciitis. Plantar fasciitis is a stretching of the plantar fascia, a ligament that runs from the ball of foot through the arch and is attached to the heel. It is that attachment which becomes aggravated and typically causes pain after being on your feet for lengths of time. Abnormal motion of the foot (pronation) is one cause of plantar fasciitis. Heel spurs, which are abnormal bone growths coming off the heel, can also cause heel pain. Other causes include repetitive stress or shock to the heel, standing for prolonged periods or osteoarthritis. To prevent heel pain, always wear properly fitting shoes, place insoles or inserts in your shoes to help control abnormal foot motion, maintain a healthy weight, exercise and do foot stretches as they have been shown to decrease the incidence of heel pain.
Causes
Plantar fasciitis is caused by inflammation and irritation of the tight tissue forming the arch of the foot. The most common cause of heel pain, it typically affects men, aged 40 - 70 who are physically active. The bottom or inside of the foot and / or heel (where heel and arch meet) may hurt or cause severe pain upon standing after resting -- or most often, when arising in the morning. The pain is usually experienced within the first few steps and is often characterized as "walking on nails" or knife blades. The pain may let up after walking a bit but most commonly returns after prolonged movement or a rest.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
If the plantar fasciitis is acute, that is, a sprain of the plantar fascia then it is basically treated as a sprain, with anti-inflammatory drugs, ice, rest, possibly physical therapy. If chronic, the poor foot mechanics need be addressed. Foot mechanics are changed by use of specially moulded shoe inserts known as orthotics. Someone with plantar fasciitis needs an orthotic designed to relieve strain on the plantar fascia. Orthotics are often confused with arch supports. Arch supports, by holding up the arch can remove some of the tension from the plantar fascia. Orthotics, on the other hand, do most of their work on the heel and ball of the foot repositioning the foot for maximized function. What can you do before you see the foot doctor? First, try doing your own version of deep tissue massage by rolling a frozen cola bottle or can from the heel forward into the arch. Do it gently. Do stretching but the key to good stretching is not to stretch too hard so generally avoid weight bearing (standing) stretches but sit on a soft surface like your bed and pull the foot backward on the leg as far as it will go, holding for 20 seconds and relaxing for 5 seconds. Each 25 second ?set? can be repeated 5 times and you have invested about 2 minutes in giving yourself a lot of help. Watch out for the shoes you wear. It is tempting to obtain shoes that are colorful and soft. Here is the proof that soft shoes are bad. Wrap a pillow around your foot with duct tape and walk for a block or two. You will come back with your foot hurting more because your foot sank down deeper into the soft surface, allowing the ligament to stretch more. The shoes should be stiff in the shank and flexible at the ball. Such shoes, to running buffs, are known as motion control shoes or stability shoes so going to one of the small specialty running shoes stores is a good place to start. If you don?t have a desk job, or have an industrial job see if light duty is available. A note from your doc may be all that is required in most cases and most doctors are happy to oblige.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
heel cushions for plantar fasciitis
Prevention

Before you get out of bed in the morning, and then periodically throughout the day, do the following exercises to increase flexibility and ease pain. Slowly flex your foot and toes to stretch the tissue on the bottom of your sore foot. Hold the stretch for 10 counts. Relax and repeat. Do gentle ankle rolls to keep the tissues around the ankle and on the back of the heel flexible. Sit on the edge of your bed and roll your foot back and forth over a tennis ball.
Shoe Lifts For Leg Length Discrepancy
Overview
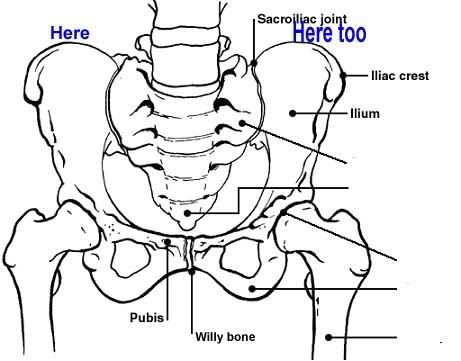
The two major categorizations of LLD are structural and functional. A third more minor category is environmental. In structural LLD there is an actual anatomical difference in the bones of the lower extremities where one side becomes shorter than the other. This type of LLD may be genetic, where the person is born in this way. In other cases it may be due to injury or infection through the growth phases of early childhood or adolescence. Some spinal abnormalities like scoliosis can also cause this condition. Functional LLD is where the bones are not the cause of difference but a muscle or pelvic condition has the effect of weakening the leg on one side. Conditions that can cause this are muscle inflexibility, adduction contractures and pelvic obliquity (amongst others). The third less severe category of environmental LLD is caused by discrepancies in the surface that the feet and legs are resting or walking on. Banked, uneven or curved surfaces can all cause environmental LLD. In LLD the asymmetric nature of the legs in relation to hips and back caused the centre of gravity to shift from its natural position. This then results in the body attempting to compensate by either tilting the pelvic areas towards the shorter side, increased knee flexing on the longer side, flexion of the ankle plantar and foot supination towards the shorter side.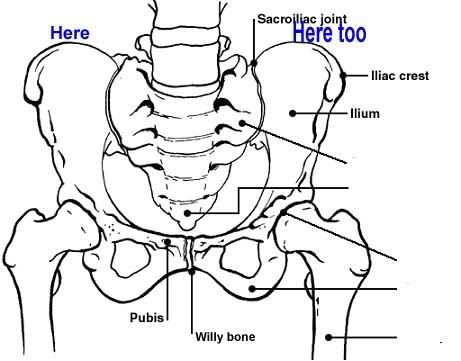
Causes
Some children are born with absence or underdeveloped bones in the lower limbs e.g., congenital hemimelia. Others have a condition called hemihypertrophy that causes one side of the body to grow faster than the other. Sometimes, increased blood flow to one limb (as in a hemangioma or blood vessel tumor) stimulates growth to the limb. In other cases, injury or infection involving the epiphyseal plate (growth plate) of the femur or tibia inhibits or stops altogether the growth of the bone. Fractures healing in an overlapped position, even if the epiphyseal plate is not involved, can also cause limb length discrepancy. Neuromuscular problems like polio can also cause profound discrepancies, but thankfully, uncommon. Lastly, Wilms? tumor of the kidney in a child can cause hypertrophy of the lower limb on the same side. It is therefore important in a young child with hemihypertrophy to have an abdominal ultrasound exam done to rule out Wilms? tumor. It is important to distinguish true leg length discrepancy from apparent leg length discrepancy. Apparent discrepancy is due to an instability of the hip, that allows the proximal femur to migrate proximally, or due to an adduction or abduction contracture of the hip that causes pelvic obliquity, so that one hip is higher than the other. When the patient stands, it gives the impression of leg length discrepancy, when the problem is actually in the hip.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
The key to treatment of LLD in a child is to predict what the discrepancy is at maturity. If it is predicted to be less than 2 cm., no treatment is needed. Limb length discrepancies of up to 2 or 2.5 cm. can be compensated very well with a lift in the shoe. Beyond 2.5 cm., it becomes increasingly difficult to compensate with a left in the insole. Building up the shoe becomes uncosmetic and cumbersome, and some other way of compensating for the discrepancy becomes necessary. The treatment of LLD is long-term treatment, and involves the physician and patient?s family working together as a team. The family needs to weigh the various options available. If leg lengthening is decided on, the family needs to understand the commitment necessary to see it through. The treatment takes 6 months to a year for completion, and complications can happen. But when it works, the results are gratifying.

how do you get taller in a day?
Surgical Treatment
Surgical treatments vary in complexity. Sometimes the goal of surgery is to stop the growth of the longer limb. Other times, surgeons work to lengthen the shorter limb. Orthopedic surgeons may treat children who have limb-length conditions with one or a combination of these surgical techniques. Bone resection. An operation to remove a section of bone, evening out the limbs in teens or adults who are no longer growing. Epiphyseal stapling. An operation to slow the rate of growth of the longer limb by inserting staples into the growth plate, then removing them when the desired result is achieved. Epiphysiodesis. An operation to slow the rate of growth of the longer limb by creating a permanent bony ridge near the growth plate. Limb lengthening. A procedure (also called distraction osteogenesis or the Ilizarov procedure) that involves attaching an internal or external fixator to a limb and gradually pulling apart bone segments to grow new bone between them. There are several ways your doctor can predict the final LLD, and thus the timing of the surgery. The easiest way is the so-called Australian method, popularised by Dr. Malcolm Menelaus, an Australian orthopedic surgeon. According to this method, growth in girls is estimated to stop at age 14, and in boys at age 16 years. The femur grows at the rate of 10 mm. a year, and the upper tibia at the rate of 6 mm. a year. Using simple arithmetic, one can get a fairly good prediction of future growth. This of course, is an average, and the patient may be an average. To cut down the risk of this, the doctor usually measures leg length using special X-ray technique (called a Scanogram) on three occasions over at least one year duration to estimate growth per year. He may also do an X-ray of the left hand to estimate the bone age (which in some cases may differ from chronological age) by comparing it with an atlas of bone age. In most cases, however, the bone age and chronological age are quite close. Another method of predicting final LLD is by using Anderson and Green?s remaining growth charts. This is a very cumbersome method, but was till the 1970?s, the only method of predicting remaining growth. More recently, however, a much more convenient method of predicting LLD was discovered by Dr. Colin Moseley from Montreal. His technique of using straight line graphs to plot growth of leg lengths is now the most widely used method of predicting leg length discrepancy. Whatever method your doctor uses, over a period of one or two years, once he has a good idea of the final LLD, he can then formulate a plan to equalize leg lengths. Epiphyseodesis is usually done in the last 2 to 3 years of growth, giving a maximum correction of about 5 cm. Leg lengthening can be done at any age, and can give corrections of 5 to10 cm., or more.
The two major categorizations of LLD are structural and functional. A third more minor category is environmental. In structural LLD there is an actual anatomical difference in the bones of the lower extremities where one side becomes shorter than the other. This type of LLD may be genetic, where the person is born in this way. In other cases it may be due to injury or infection through the growth phases of early childhood or adolescence. Some spinal abnormalities like scoliosis can also cause this condition. Functional LLD is where the bones are not the cause of difference but a muscle or pelvic condition has the effect of weakening the leg on one side. Conditions that can cause this are muscle inflexibility, adduction contractures and pelvic obliquity (amongst others). The third less severe category of environmental LLD is caused by discrepancies in the surface that the feet and legs are resting or walking on. Banked, uneven or curved surfaces can all cause environmental LLD. In LLD the asymmetric nature of the legs in relation to hips and back caused the centre of gravity to shift from its natural position. This then results in the body attempting to compensate by either tilting the pelvic areas towards the shorter side, increased knee flexing on the longer side, flexion of the ankle plantar and foot supination towards the shorter side.
Causes
Some children are born with absence or underdeveloped bones in the lower limbs e.g., congenital hemimelia. Others have a condition called hemihypertrophy that causes one side of the body to grow faster than the other. Sometimes, increased blood flow to one limb (as in a hemangioma or blood vessel tumor) stimulates growth to the limb. In other cases, injury or infection involving the epiphyseal plate (growth plate) of the femur or tibia inhibits or stops altogether the growth of the bone. Fractures healing in an overlapped position, even if the epiphyseal plate is not involved, can also cause limb length discrepancy. Neuromuscular problems like polio can also cause profound discrepancies, but thankfully, uncommon. Lastly, Wilms? tumor of the kidney in a child can cause hypertrophy of the lower limb on the same side. It is therefore important in a young child with hemihypertrophy to have an abdominal ultrasound exam done to rule out Wilms? tumor. It is important to distinguish true leg length discrepancy from apparent leg length discrepancy. Apparent discrepancy is due to an instability of the hip, that allows the proximal femur to migrate proximally, or due to an adduction or abduction contracture of the hip that causes pelvic obliquity, so that one hip is higher than the other. When the patient stands, it gives the impression of leg length discrepancy, when the problem is actually in the hip.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
The key to treatment of LLD in a child is to predict what the discrepancy is at maturity. If it is predicted to be less than 2 cm., no treatment is needed. Limb length discrepancies of up to 2 or 2.5 cm. can be compensated very well with a lift in the shoe. Beyond 2.5 cm., it becomes increasingly difficult to compensate with a left in the insole. Building up the shoe becomes uncosmetic and cumbersome, and some other way of compensating for the discrepancy becomes necessary. The treatment of LLD is long-term treatment, and involves the physician and patient?s family working together as a team. The family needs to weigh the various options available. If leg lengthening is decided on, the family needs to understand the commitment necessary to see it through. The treatment takes 6 months to a year for completion, and complications can happen. But when it works, the results are gratifying.

how do you get taller in a day?
Surgical Treatment
Surgical treatments vary in complexity. Sometimes the goal of surgery is to stop the growth of the longer limb. Other times, surgeons work to lengthen the shorter limb. Orthopedic surgeons may treat children who have limb-length conditions with one or a combination of these surgical techniques. Bone resection. An operation to remove a section of bone, evening out the limbs in teens or adults who are no longer growing. Epiphyseal stapling. An operation to slow the rate of growth of the longer limb by inserting staples into the growth plate, then removing them when the desired result is achieved. Epiphysiodesis. An operation to slow the rate of growth of the longer limb by creating a permanent bony ridge near the growth plate. Limb lengthening. A procedure (also called distraction osteogenesis or the Ilizarov procedure) that involves attaching an internal or external fixator to a limb and gradually pulling apart bone segments to grow new bone between them. There are several ways your doctor can predict the final LLD, and thus the timing of the surgery. The easiest way is the so-called Australian method, popularised by Dr. Malcolm Menelaus, an Australian orthopedic surgeon. According to this method, growth in girls is estimated to stop at age 14, and in boys at age 16 years. The femur grows at the rate of 10 mm. a year, and the upper tibia at the rate of 6 mm. a year. Using simple arithmetic, one can get a fairly good prediction of future growth. This of course, is an average, and the patient may be an average. To cut down the risk of this, the doctor usually measures leg length using special X-ray technique (called a Scanogram) on three occasions over at least one year duration to estimate growth per year. He may also do an X-ray of the left hand to estimate the bone age (which in some cases may differ from chronological age) by comparing it with an atlas of bone age. In most cases, however, the bone age and chronological age are quite close. Another method of predicting final LLD is by using Anderson and Green?s remaining growth charts. This is a very cumbersome method, but was till the 1970?s, the only method of predicting remaining growth. More recently, however, a much more convenient method of predicting LLD was discovered by Dr. Colin Moseley from Montreal. His technique of using straight line graphs to plot growth of leg lengths is now the most widely used method of predicting leg length discrepancy. Whatever method your doctor uses, over a period of one or two years, once he has a good idea of the final LLD, he can then formulate a plan to equalize leg lengths. Epiphyseodesis is usually done in the last 2 to 3 years of growth, giving a maximum correction of about 5 cm. Leg lengthening can be done at any age, and can give corrections of 5 to10 cm., or more.
What Is Mortons Neuroma
Overview
 Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.
Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.
Causes
Morton's neuroma develops for several reasons. The primary reason is wearing narrow toe-box shoes, which compress the metatarsal heads. Certain anatomical factors also make nerve compression more likely with the narrow toe box shoes. In some people fibers, the medial and lateral plantar nerves converge close to the heads of the third and fourth metatarsals. This junction creates a larger nerve structure between the metatarsal heads making it more vulnerable to compression.
Symptoms
Often, no outward signs (such as a lump or unusual swelling) appear from the condition. Neuroma pain is most often described as a burning discomfort in the forefoot. Aching or sudden shooting pain in the forefoot is also common. All running sports, especially distance running can leave an athlete vulnerable to Morton?s Neuroma, which may appear or flare up in the middle of a run or at the end. The sufferer often has the desire to remove his shoe and rub the afflicted foot. Should the Neuroma be of sufficient size, or if footwear is particularly tight or uncomfortable, the painful condition may be present during normal walking. Numbness in the foot may precede or accompany Neuroma pain.
Diagnosis
The diagnosis of interdigital neuroma is usually made by physical examination and review of the patient's medical history.MRI ad High Definition Ultrasound examination may be useful to confirm the diagnoses however they may still not be 100% reliable. The commonest reason for this is de to natural substances present in between the metatarsal heads and between the fat pad and the intermetatarsal ligament. These natural substances i.e. bursa, fat, capsular thickening and even bony growths, can all be a factor in the impingement process and may need to be surgically cleared.
Non Surgical Treatment
Wear shoes with plenty of room for the toes to move, low heels, and laces or buckles that allow for width adjustment. Wear shoes with thick, shock-absorbent soles, as well as proper insoles that are designed to keep excessive pressure off of the foot. High-heeled shoes over two inches tall should be avoided whenever possible because they place undue strain on the forefoot. Resting the foot and massaging the affected area can temporarily alleviate neuroma pain. Use an ice pack to help to dull the pain and improve comfort. Use over-the-counter shoe pads. These pads can relieve pressure around the affected area.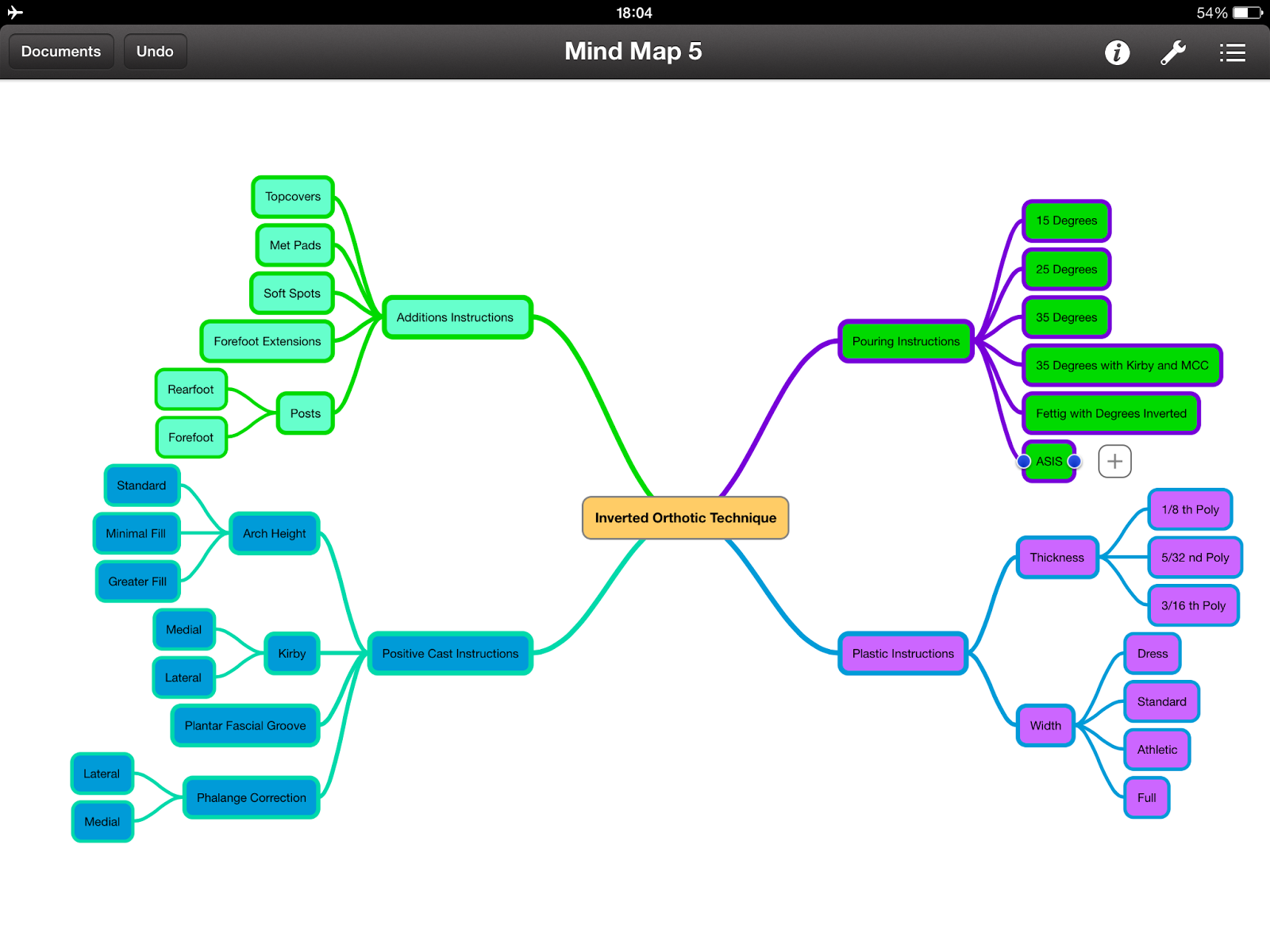
Surgical Treatment
If these non-surgical measures do not work, surgery is sometimes needed. Surgery normally involves a small incision (cut) being made on either the top, or the sole, of the foot between the affected toes. Usually, the surgeon will then either create more space around the affected nerve (known as nerve decompression) or will cut out (resect) the affected nerve. If the nerve is resected, there will be some permanent numbness of the skin between the affected toes. This does not usually cause any problems. You will usually have to wear a special shoe for a short time after surgery until the wound has healed and normal footwear can be used again. Surgery is usually successful. However, as with any surgical operation, there is a risk of complications. For example, after this operation a small number of people can develop a wound infection. Another complication may be long-term thickening of the skin (callus formation) on the sole of the foot (known as plantar keratosis). This may require treatment by a specialist in care of the feet (chiropody).
 Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.
Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.Causes
Morton's neuroma develops for several reasons. The primary reason is wearing narrow toe-box shoes, which compress the metatarsal heads. Certain anatomical factors also make nerve compression more likely with the narrow toe box shoes. In some people fibers, the medial and lateral plantar nerves converge close to the heads of the third and fourth metatarsals. This junction creates a larger nerve structure between the metatarsal heads making it more vulnerable to compression.
Symptoms
Often, no outward signs (such as a lump or unusual swelling) appear from the condition. Neuroma pain is most often described as a burning discomfort in the forefoot. Aching or sudden shooting pain in the forefoot is also common. All running sports, especially distance running can leave an athlete vulnerable to Morton?s Neuroma, which may appear or flare up in the middle of a run or at the end. The sufferer often has the desire to remove his shoe and rub the afflicted foot. Should the Neuroma be of sufficient size, or if footwear is particularly tight or uncomfortable, the painful condition may be present during normal walking. Numbness in the foot may precede or accompany Neuroma pain.
Diagnosis
The diagnosis of interdigital neuroma is usually made by physical examination and review of the patient's medical history.MRI ad High Definition Ultrasound examination may be useful to confirm the diagnoses however they may still not be 100% reliable. The commonest reason for this is de to natural substances present in between the metatarsal heads and between the fat pad and the intermetatarsal ligament. These natural substances i.e. bursa, fat, capsular thickening and even bony growths, can all be a factor in the impingement process and may need to be surgically cleared.
Non Surgical Treatment
Wear shoes with plenty of room for the toes to move, low heels, and laces or buckles that allow for width adjustment. Wear shoes with thick, shock-absorbent soles, as well as proper insoles that are designed to keep excessive pressure off of the foot. High-heeled shoes over two inches tall should be avoided whenever possible because they place undue strain on the forefoot. Resting the foot and massaging the affected area can temporarily alleviate neuroma pain. Use an ice pack to help to dull the pain and improve comfort. Use over-the-counter shoe pads. These pads can relieve pressure around the affected area.
Surgical Treatment
If these non-surgical measures do not work, surgery is sometimes needed. Surgery normally involves a small incision (cut) being made on either the top, or the sole, of the foot between the affected toes. Usually, the surgeon will then either create more space around the affected nerve (known as nerve decompression) or will cut out (resect) the affected nerve. If the nerve is resected, there will be some permanent numbness of the skin between the affected toes. This does not usually cause any problems. You will usually have to wear a special shoe for a short time after surgery until the wound has healed and normal footwear can be used again. Surgery is usually successful. However, as with any surgical operation, there is a risk of complications. For example, after this operation a small number of people can develop a wound infection. Another complication may be long-term thickening of the skin (callus formation) on the sole of the foot (known as plantar keratosis). This may require treatment by a specialist in care of the feet (chiropody).
The Answer To Leg Length Imbalances Is Shoe Lifts
There are not one but two different types of leg length discrepancies, congenital and acquired. Congenital implies you are born with it. One leg is structurally shorter in comparison to the other. Through developmental periods of aging, the brain picks up on the stride pattern and identifies some variation. The entire body usually adapts by dipping one shoulder over to the "short" side. A difference of under a quarter inch isn't really abnormal, doesn't need Shoe Lifts to compensate and commonly won't have a profound effect over a lifetime.

Leg length inequality goes typically undiscovered on a daily basis, however this problem is simply solved, and can reduce a number of cases of lumbar pain.
Treatment for leg length inequality commonly consists of Shoe Lifts . They are affordable, normally priced at below twenty dollars, compared to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Low back pain is the most prevalent condition affecting men and women today. Over 80 million people suffer from back pain at some point in their life. It is a problem which costs employers vast amounts of money yearly on account of lost time and production. New and superior treatment solutions are continually sought after in the hope of decreasing the economical impact this condition causes.

Men and women from all corners of the world suffer the pain of foot ache as a result of leg length discrepancy. In these cases Shoe Lifts can be of worthwhile. The lifts are capable of relieving any discomfort and pain in the feet. Shoe Lifts are recommended by many expert orthopaedic orthopedists.
So as to support the human body in a healthy and balanced manner, your feet have a crucial task to play. Irrespective of that, it is often the most overlooked area of the human body. Some people have flat-feet which means there is unequal force exerted on the feet. This will cause other body parts including knees, ankles and backs to be impacted too. Shoe Lifts guarantee that ideal posture and balance are restored.

Leg length inequality goes typically undiscovered on a daily basis, however this problem is simply solved, and can reduce a number of cases of lumbar pain.
Treatment for leg length inequality commonly consists of Shoe Lifts . They are affordable, normally priced at below twenty dollars, compared to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Low back pain is the most prevalent condition affecting men and women today. Over 80 million people suffer from back pain at some point in their life. It is a problem which costs employers vast amounts of money yearly on account of lost time and production. New and superior treatment solutions are continually sought after in the hope of decreasing the economical impact this condition causes.

Men and women from all corners of the world suffer the pain of foot ache as a result of leg length discrepancy. In these cases Shoe Lifts can be of worthwhile. The lifts are capable of relieving any discomfort and pain in the feet. Shoe Lifts are recommended by many expert orthopaedic orthopedists.
So as to support the human body in a healthy and balanced manner, your feet have a crucial task to play. Irrespective of that, it is often the most overlooked area of the human body. Some people have flat-feet which means there is unequal force exerted on the feet. This will cause other body parts including knees, ankles and backs to be impacted too. Shoe Lifts guarantee that ideal posture and balance are restored.
Caring For Inferior Calcaneal Spur

Overview
If you're feeling pain on the bottom of your foot near your heel, pain after exercise or activity, or pain first thing in the morning or after a long period of sitting, then you may have a heel spur. Heel spurs don't have a magic cure, but you can take steps to ease the pain and to eventually get rid of them.
Causes
A major cause of heel spur pain comes from the development of new fibrous tissue around the bony spur, which acts as a cushion over the area of stress. As this tissue grows, a callus forms and takes up even more space than the heel spur, leading to less space for the thick surrounding network of tendons, nerves, ligaments and supporting tissue. These important structures in the foot have limited space because of calcium or tissue buildup, which leads to swelling and redness of the foot, and a deep throbbing pain worsened with exercise.

Symptoms
The Heel Spur itself is not thought to be painful. Patients who experience pain with Plantar Fasciitis are suffering from inflammation and irritation of the plantar fascia. This the primary cause of pain and not the Heel Spur. Heel Spurs form in some patients who have plantar fasciitis, and tend to occur in patients who have had the problem for a prolonged period of time. While about 70 % of patients with plantar fasciitis have a heel spur, X-rays also show about 50 % of patients with no symptoms of plantar fasciitis also have a heel spur.
Diagnosis
Heel spurs and plantar fasciitis is usually diagnosed by your physiotherapist or sports doctor based on your symptoms, history and clinical examination. After confirming your heel spur or plantar fasciitis they will investigate WHY you are likely to be predisposed to heel spurs and develop a treatment plan to decrease your chance of future bouts. X-rays will show calcification or bone within the plantar fascia or at its insertion into the calcaneus. This is known as a calcaneal or heel spur. Ultrasound scans and MRI are used to identify any plantar fasciitis tears, inflammation or calcification. Pathology tests may identify spondyloarthritis, which can cause symptoms similar to plantar fasciitis.
Non Surgical Treatment
A conventional treatment for a heel spur is a steroid injection. This treatment, however, isn?t always effective because of the many structures in the heel, making it a difficult place for an injection. If this treatment goes wrong, it can make the original symptoms even worse. Another interesting means of treatment is Cryoultrasound, an innovative electromedical device that utilizes the combination of two therapeutic techniques: cryotherapy and ultrasound therapy. Treatments with Cryoultrasound accelerate the healing process by interrupting the cycle and pain and spasms. This form of therapy increases blood circulation and cell metabolism; it stimulates toxin elimination and is supposed to speed up recovery.
Surgical Treatment
Almost 90% of the people suffering from heel spur get better with nonsurgical treatments. However, if the conservative treatments do not help you and you still have pain even after 9 to 12 months, your doctor may advise surgery for treating heel spur. The surgery helps in reducing the pain and improving your mobility. Some of the surgical techniques used by doctors are release of the plantar fascia. Removal of a spur. Before the surgery, the doctor will go for some pre-surgical tests and exams. After the operation, you will need to follow some specific recommendations which may include elevation of the foot, waiting time only after which you can put weight on the foot etc.
Prevention
Prevention of heel spur syndrome may be best by finding a good supportive shoe. Never go barefoot or wear a flat soled shoe. There are many over the counter arch supports that give increased support for your feet. Usually when there is excessive pronation the Achilles Tendon contracts or becomes shortened over time since it is not being used fully. The shortened Achilles Tendon is called an equinus deformity. By keeping this tendon stretched it may decrease some of the tension in the foot. Some theories believe the Achilles Tendon and plantar fascia is continuous. Before you get up from rest, stretch out your Achilles and the plantar fascia. You may attempt to spell the alphabet with your foot and ankle, use a towel against pressure on your foot, or roll a can of soup or sodapop on the ground. Ice may work well at the times of severe pain. For a chronic pain, or longer lasting pain heat therapy may improve the condition.
Have I Got Inferior Calcaneal Spur

Overview
The heel bone is the largest bone in the foot and absorbs the most shock and pressure. A heel spur develops as an abnormal growth of the heel bone. Most commonly, calcium deposits form when the plantar fascia pulls away from the heel area, causing a bony protrusion, or heel spur to develop. While bone spurs can develop in other locations such as the rear of the heel bone, this is the most common location for development. The plantar fascia is a broad band of fibrous tissue located along the bottom surface of the foot that runs from the heel to the forefoot. Heel spurs can cause extreme pain in the rearfoot, especially while standing or walking.
Causes
When a patient has plantar fasciitis, the plantar fascia becomes inflamed and degenerative (worn out)--these abnormalities can make normal activities quite painful. Symptoms typically worsen early in the morning after sleep. At that time, the plantar fascia is tight so even simple movements stretch the contracted plantar fascia. As you begin to loosen the plantar fascia, the pain usually subsides, but often returns with prolonged standing or walking.

Symptoms
Most heel spurs cause no symptoms and may go undetected for years. If they cause no pain or discomfort, they require no treatment. Occasionally, a bone spur will break off from the larger bone, becoming a ?loose body?, floating in a joint or embedding itself in the lining of the joint. This can cause pain and intermittent locking of the joint. In the case of heel spurs, sharp pain and discomfort is felt on the bottom of the foot or heel.
Diagnosis
Diagnosis is made using a few different technologies. X-rays are often used first to ensure there is no fracture or tumor in the region. Then ultrasound is used to check the fascia itself to make sure there is no tear and check the level of scar tissue and damage. Neurosensory testing, a non-painful nerve test, can be used to make sure there is not a local nerve problem if the pain is thought to be nerve related. It is important to remember that one can have a very large heel spur and no plantar fasciitis issues or pain at all, or one can have a great deal of pain and virtually no spur at all.
Non Surgical Treatment
Acupuncture and acupressure can used to address the pain of heel spurs, in addition to using friction massage to help break up scar tissue and delay the onset of bony formations. Physical therapy may help relieve pain and improve movement. The Feldenkrais method could be especially helpful for retraining some of the compensation movements caused by the pain from the spur. Guided imagery or a light massage on the foot may help to relieve some of the pain. Other treatments include low-gear cycling, and pool running. Some chiropractors approve of moderate use of aspirin or ibuprofen, or other appropriate anti-inflammatory drugs. Chiropractic manipulation is not recommended, although chiropractors may offer custom-fitted shoe orthotics and other allopathic-type treatments.
Surgical Treatment
Surgery is used a very small percentage of the time. It is usually considered after trying non-surgical treatments for at least a year. Plantar fascia release surgery is use to relax the plantar fascia. This surgery is commonly paired with tarsal tunnel release surgery. Surgery is successful for the majority of people.